Canine Education
Allergies
What is an Allergy?
Allergy is a state of hypersensitivity in which exposure to a harmless substance known as an allergen induces the body’s immune system to “overreact.” Dogs usually manifest their allergies or hypersensitivities in the form of skin disease, as opposed to people who usually display symptoms of respiratory disease or “hay fever” (watery eyes, runny nose, sneezing). This will often present as the “itchy” patient or the patient with skin disease resulting from self-excoriation and secondary skin infections. The 3 most common allergens to affect canines are: flea allergy, airborne allergy (this will be referred to as “atopy” hereafter), and food allergy. Each of these will be discussed in further detail. Allergies to all of the above usually result in some form of itching, licking, or chewing of the skin. Skin allergies can be very difficult to manage, and even with the best care, many dogs will still experience some degree of itchiness. Unfortunately, we are not usually able to “cure” allergies and this is typically a life-long problem that your dog may experience in varying degrees throughout the year. Our goal is to control allergies as best as possible to improve the quality of life for you and your pet.
Read below for more information about the major types of allergies that affect dogs.
Flea Allergy (Flea Allergy Dermatitis)
Flea allergy dermatitis or FAD is the most common allergy affecting both dogs and cats. Many animals have flea infestations with minimal to no skin disease, while animals with FAD can have profound skin disease with the presence of very few fleas. The allergy is caused by an individual patient’s hypersensitivity to the flea saliva and it only takes a few bites to induce the problem. For this reason, very regular flea control is essential to help keep FAD animals symptom-free. The itching and skin disease associated with flea allergy is most commonly distributed around the base of the tail, along the back, down the back legs and on the stomach. Hair loss or thinning is often present in those areas and the skin may be red, crusty and have red bumps called papules. The goal to prevent the itchiness associated with FAD is regular flea control. But, sometimes in order to control severe itchiness we may recommend oral steroids. This will depend on the severity of your dog’s current flare up.
I don’t understand…I never see fleas on my dog. How can the problem be flea related?
You may not see them, but that doesn’t mean they aren’t there. Due to our hot, humid climate, fleas are EVERYWHERE in Louisiana. Again, it only takes a few bites to induce the problem. One trip into a flea infested environment can result in several flea bites even in dogs that are on appropriate flea prevention. Also, the itchy pet often scratches and bites so much that adult fleas are removed, making them hard to find.
How often must flea prevention be given?
If you have a dog affected with FAD, then monthly, year-round prevention is essential to help control symptoms. We have both oral and topical preventatives available. Please ask a member of our staff for our best current recommendation.
Atopy or Airborne Allergy (Atopic Dermatitis)
Atopic dermatitis (AD) is an inherited predisposition to develop itchiness and skin disease from exposure to a variety of commonplace and otherwise harmless substances including dust, mold spores, and the pollens of weeds, grasses and trees. Symptoms may be seasonal in some patients, but the absence of a seasonal component does not rule out atopy as the cause of your dog’s itchiness. Diagnosis of AD is usually made on suspicion from the patient’s history, clinical presentation and response to treatment. A more specific diagnosis can be made using intradermal skin testing, but this is not available in most general vet practices and usually requires referral to a veterinary dermatologist. The vet will discuss this with you if he/she feels it is warranted. The skin disease and itchiness associated with atopy can exist on almost any part of the body but the following areas are most common: feet, face, lower chest or abdomen, arm pits, and ears. Affected areas may be red, crusty, have a thinned hair coat and may contain red bumps called papules. These skin changes are usually the result of self trauma from scratching, licking or chewing. Secondary infections with bacteria and/or yeast are very common. Ear infections also commonly accompany AD and some animals may have this as their sole manifestation of the allergy.
How can atopic dermatitis be managed?
Antihistamines (Benadryl, Chlorpheniramine, Zertec, etc.) are often used as a first line of defense. Unfortunately, antihistamines are often minimally effective against the itchiness that accompanies atopy. Because of their safety with long-term use, low degree of side effects, and accessibility, antihistamines are still often tried. The vet will speak with you about dosing options for your dog.
Steroids (Prednisone, Dexamethasone, DepoMedrol, etc) are usually very effective in controlling atopy but their use must be limited due to side effects, especially with long-term use. The most common side effects are increased thirst, increased urination, increased appetite, and panting. Steroids are an immunosuppressive medication and do increase the risk of acquiring infections. Long-term use is rarely advised as a control for atopy and owners must understand the possible risks. Most patients are started on a higher dose then tapered or decreased to a lower dose over time.
Reducing Exposure to the Allergen The following are general tips to avoid exposure that can be practiced; although, in the dog with moderate to severe atopy, even strict adherence to these guidelines may not resolve symptoms.
- Weekly baths to remove allergens from skin surface. Careful to avoid over bathing, as atopic dogs are subject to drying of the skin. There are many good OTC hydrating shampoos. Bathes and/or washing of the feet after prolonged trips outside may help.
- Wash bedding regularly. Vacuum regularly and keep pet away when dusting, vacuuming or cutting the grass.
- Use air conditioning and/or air filter system
Omega 3 Fatty Acid Supplementation may help to decrease the severity of symptoms or help to decrease the frequency of needed medication. These products are NOT analogous to adding oil to the pet’s food. There are many good OTC products available. It often takes 6 weeks to build up enough omega 3 fatty acids in the body to observe a difference.
Hyposensitization (Allergy Shots) These injections are available for canines, but formulation is based on intradermal skin testing, which currently requires referral to a veterinary dermatologist. The vet can speak with you more about this if you are interested.
Food Allergy (FA)
Some pets develop specific hypersensitivities to components of their diets. The allergen is usually a major protein or carbohydrate ingredient such as beef, chicken, pork, corn, wheat, or soy. Minor ingredients such as preservatives or dyes are also potential allergens. The skin disease and itchiness associated with FA can exist on almost any part of the body but these are most common: face, feet, lower abdomen, ears, and anus. Affected areas may be red, crusty, have a thinned hair coat and may contain red bumps called papules. These skin changes are usually the result of self trauma from scratching, licking or chewing. Secondary infections with bacteria and/or yeast are very common. Ear infections also commonly accompany FA and some animals may have this as their sole manifestation of the allergy.
How can food allergy be diagnosed?
A food trial is performed, which means that we test your pet by feeding a special, strict diet that contains only ingredients that the patient has never eaten before. This is often achieved by feeding a prescription diet for a period of 10 to 16 weeks. If the signs resolve after this period, a challenge is performed by feeding the former diet and watching for a return of the itching. If this occurs, a diagnosis of food allergy is confirmed. The vet can speak in more detail about these diets.
But my dog has been eating this food for a long time? Why now?
Many people assume that the itching due to FA requires a recent diet change, but the opposite is often true. FA takes time to develop; most animals have been eating the offending food for years with no trouble.
Combined Allergies
Some animals have multiple allergies. It would not be particularly unusual for an animal with atopy or food allergy to also be allergic to fleas, especially considering that flea bite allergy is extremely common among pets. Because allergies add to each other, it is possible that an atopic or food allergic dog will not itch as long as its fleas are controlled. This is why we will always stress the importance of flea preventative in any dog with allergic skin disease. Since new technology has made flea control safe and convenient, it is especially important to ensure that fleas are not complicating a pet’s itching problem.
Heartworm Disease
What is Heartworm Disease?

Heartworm disease is a serious and potentially fatal condition caused by parasitic worms living in the arteries that take blood from the heart to the lungs and the right side of the heart. Pictured is an illustration of what this looks like in a canine heart. Heartworm disease has been reported in all 50 states; however, the southeastern United States is where the vast majority of heartworm positive cases are reported. Therefore, any dogs not on heartworm prevention in Louisiana are at a very high risk of contracting the disease.
Life Cycle
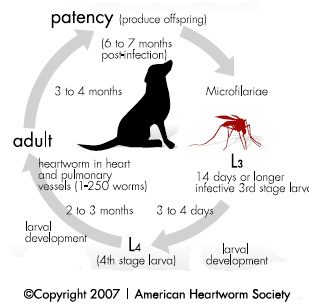
The basic life cycle of the heartworm is: mosquito contracts heartworms from biting a dog that has heartworms, and then the mosquito bites another dog and gives it to that dog. We frequently are asked if heartworms is contagious, and the answer to that question is “no”. Dogs can only get heartworms from a mosquito that has heartworms. For all intensive purposes the heartworms in the mosquito are “baby” heartworms (AKA microfilariae). When a mosquito with baby heartworms bites a dog it injects the baby heartworms into the dog. After about 2-3 months the baby heartworms mature into adults. Approximately 6-7 months after infection the adult heartworms begin to reproduce and the cycle begins again.
Clinical Signs (Symptoms)
The majority of heartworm positive dogs do not have clinical signs. This is because testing is performed yearly and typically cases are diagnosed early in the course of the disease. When clinical signs exist, coughing and/or exercise intolerance are most commonly observed. As the disease progresses patients begin to lose weight, become more lethargic, can sometimes faint or collapse, and can even develop right-sided congestive heart failure. Right-sided congestive heart failure typically causes fluid accumulation within the abdomen or within the skin and jugular vein distention. The most severe and life threatening cases are at the “end-stage” of the disease, which we refer to as caval syndrome. In caval syndrome the patient will typically have discolored urine, a heart murmur, right-sided and possibly left-sided congestive heart failure, and rapid or difficulty breathing. Most patients in caval syndrome do not survive.
Treatment
Treatment for heartworm disease consists of a series of injections, with a medication called Melarsomine, given in the lower back muscles. There are two options: either a two-injection series or three-injection series. The primary difference between them is the safety, effectiveness, time-frame, and cost. Regardless of the option chosen we recommend that all patients treated be started on Proheart 6 for heartworm prevention at minimum one month prior to beginning treatment.
Two-Injection Series
With the two injection series patients receive one injection on two consecutive days. They receive the first injection on the morning they arrive, spend the night, and then receive the second injection the following morning. Following the injections the patients return in two weeks for a heart and lung check, and again two weeks after that (four weeks post-treatment) for microfilariacide, which is treatment given by mouth to ensure that all baby heartworms are killed. Once this is completed the patient is finished with treatment and will be retested for heartworms one year post treatment.
The two-injection series is considered less effective mainly because the patient will only be receiving two injections as opposed to three; and therefore, there is greater risk that all the heartworms will not be killed. Because a two-injection series is given all at once it causes a more rapid killing of the heartworms and this could result in a clot to form from dead or dying heartworms in the arteries. A clot formation can be life threatening. In addition, the injections are hard on the patient’s body/heart and in some patients the quick administration of Melarsomine can be very taxing and possibly life threatening. That being said; we have had equal success with both the two and three injection series, and we very rarely have had complications associated with either treatment protocol. Since the two injection series requires that one less injection be given it is less expensive than the three injection series.
Three-injection Series
With the three-injection series patients receive one injection and then return one month later to receive their next two injections, which are given on two consecutive days. Following the final injection patients return in two weeks for a heart and lung check and then again two weeks after that (four weeks post final injection) for microfilariacide, which is treatment given by mouth to ensure that all baby heartworms are killed. Once this is completed the patient is finished with treatment and will be retested for heartworms one year post treatment.
The three-injection series is considered to be more effective than the two-injection series mainly because the patient will be receiving three injections as opposed to two; and therefore, there is greater chance that all heartworms will be killed. In addition, the three-injection series is considered safer because the injections are more spread out. The first injection is estimated to kill approximately 50% of the heartworms, leaving only about half to be killed at the final two injections given a month later. This “slower kill” method reduces the chances of clot formation. That being said; we have had equal success with both the two and three injection series, and we very rarely have had complications associated with either treatment protocol. The three-injection series is more expensive than the two-injection series because an additional injection is given.
Post-Treatment Care
A crucial step in a successful treatment of heartworm disease is the care given after treatment is completed. It is extremely important that patient’s activity be strictly regulated/restricted for 6-8 weeks after each injection. This means that patients should only be leach walked outside and should never be able to run freely. This also may mean that when leaving your home your pet may have to be confined to a cage or a room to prevent excessive activity. This is important because if the heart starts beating too fast and hard it can “throw a clot” of dead worms, which can be life-threatening. After treatment patients will also be prescribed steroid tablets to help reduce inflammation associated with the disease and with the treatment.
It is important to note that even when treatment is performed (no matter which protocol) patients can experience clinical signs such as coughing. This is because with heartworm disease there is a degree of permanent damage that occurs in the lungs. Many times this manifests itself as a patient who is completely healthy and normal, but when beginning excessive exercise or activity will begin coughing and even gagging. If this occurs then it is recommended to pause activity and allow patient to rest before starting again.
Prevention
Since treatment can be very financially burdensome on owners and physically burdensome on patients it is highly recommended that all patients be kept on heartworm prevention at all times. Our top choice for heartworm prevention is Proheart 6, which is an injection that patients receive every six months to prevent heartworm disease. We also offer Heartgard as a monthly preventative. If you have a pet that is not currently on heartworm prevention then we strongly recommend that you speak with any of our staff as soon as possible about getting your pet started.
Common Household Toxicities
Anticoagulant Rodenticides (Rat Poison)
Source:
95% of all rodenticides
Action:
Impedes the ability of the animal to clot blood by depleting the body of Vitamin K. Vitamin K is needed to activate certain clotting factors. Therefore, without vitamin K the body is unable to clot blood.
Clinical signs:
Blood loss resulting in anemia and other clinical signs:
i.Bleeding into chest cavity, lungs, brain, abdomen, intestines, etc.
ii.Bleeding results in shortness of breath, weakness, neurologic abnormalities, bruising on skin, and dark tarry stool among others.
Treatment:
i. If known ingestion within 4 hours then induce vomiting using syrup of ipecac or bring to veterinarian.
ii. After induction of vomiting bring pet to veterinarian as soon as possible for further treatment.
iii. Mainstay of treatment is Vitamin K injections at veterinarian and tablets at home.
This is a serious toxicity as clinical signs may not become apparent until too much blood has been lost and pet may die due to toxicity. Therefore if you notice your pet having any of these signs and there is chance of exposure they should be brought to the veterinarian immediately.
Sago Palm
Source:
Any part of plant, but seeds most toxic.
Action:
Irritation to GI tract followed neurologic abnormalities and more profoundly liver damage.
Clinical signs:
i. GI irritation: vomiting, diarrhea, anorexia (typically first signs noticed)
ii. Neurologic: difficulty walking/standing, weakness, seizures
iii. Liver damage (typically occurs a few days after ingestion): lethargy, anorexia, vomiting, prolonged clotting time, jaundice.
Treatment:
i. Induction of vomiting followed by supportive and symptomatic care
ii. Liver protectant medication Sago palms are a common plant at many households.
Most cases of toxicity occur when owner either trims or removes plant. At times the clinical signs can resolve and then later return due to liver damage.
Acetaminophen (Tylenol)
Action:
Chemical reaction causes damage to liver. This reaction also causes production of methemoglobin. Methemoglobin greatly reduces the ability the blood to deliver oxygen to tissues. Also results in the body self destructing red blood cells.
Clinical signs:
1. Blue or purple discoloration of tissue
2. Anemia (pale mucous membranes)
3. Jaundice (yellow mucous membranes)
4. Anorexia
5. Lethargy/depression
Treatment:
1. Induce vomiting with syrup of ipecac.
2. Bring pet to veterinarian as soon as possible for further therapy.
Tylenol is more toxic in cats than in dogs. As little as 1 Tylenol tablet may elicit toxicity in cats, two may be lethal. Although it is less toxic in dogs, it will still cause same effect if enough Tylenol is consumed.
Xylitol (sugar substitute)
Source:
Artificial sweetener found in sugar free gum, toothpaste, and some candies.
Action:
Causes rapid increase in insulin which greatly lowers blood sugar and also causes liver failure.
Clinical signs:
i. Low blood sugar (early onset 30-60 minutes): weakness, difficulty walking/standing, seizures, vomiting, diarrhea
ii. Liver failure (later onset 10-72 hours): lethargy, vomiting, remainder of changes are abnormalities in blood work.
Treatment:
i. IV dextrose
ii. Liver protectant drugs
iii. Monitor liver enzymes on blood work.
Treatment is typically successful if performed quickly.
Onions & Garlic
Source:
iBulb of the plant
Action:
Causes changes to red blood cell that results in self-destruction of red blood cell resulting in anemia.
Clinical signs:
i. Blue or purple discoloration of tissue
ii. Anemia
Treatment:
Do not feed your pet things with onions in them.
Grapes & Raisins
Source:
Any type of grape or raisin. Variable toxicity as some dogs eat without complications, while in other dogs can be fatal.
Action:
Unknown but results in kidney failure
Clinical signs:
i. Vomiting, anorexia, diarrhea, little to no urine production
Treatment:
i. Induce vomiting if known ingestion
ii. Supportive therapy with IV fluids
Lillies
*Only toxic to cats
Source:
Any part of plant
Action:
Two phases, but ultimately results in kidney failure
Clinical signs
i. 1st phase: vomiting, salivation, depression, anorexia – subsides within 6 hours.
ii. 2nd phase: little to no urine production, severe dehydration, kidney failure
Treatment
i. Induction of vomiting if known ingestion
ii. Supportive therapy with IV fluids
Chocolate
Source:
Different chocolates have different amounts of toxicity. In general, the darker the chocolate the more dangerous it is.
Action:
Causes increased activity of skeletal and cardiac muscle. Also causes increased central nervous system stimulation and irritability.
Clinical Signs:
i. Vomiting and/or diarrhea
ii. Restlessness, hyperactivity
iii. Increased heart rate
iv. Increased breathing rate
v. Agitation
vi. Tremors and/or seizures
vii. Difficulty walking/standing
viii. Increased urination
Treatment:
i. Induction of vomiting if known ingestion
ii. Symptomatic and supportive treatment depending on severity of symptoms
Anti-freeze (Ethylene Glycol)
Source:
Antifreeze most common
Action:
Three different phases of toxicosis:
1. Central nervous system depression
2. Profound acidosis
3. Kidney disease
Clinical signs:
i. Central nervous system depression: difficulty walking/balancing, in coordination, increased heart rate, unconsciousness
ii. Profound acidosis: fluid buildup in lungs (most common), rapid heart rate, depression/lethargy, anorexia, vomiting.
iii. Kidney disease: very little urine output to possibly no urine output, vomiting, anorexia, lethargy. – kidney disease primarily due to production urine crystals.
Treatment:
If known ingestion of toxicity or suspected ingestion pet should be brought to veterinarian immediately.
Most important is to never leave antifreeze on ground or where a pet could drink some because it is sweet in taste, but extremely toxic and life-threatening.
Poinsettia
Many people think these are highly toxic plants. However, they are rarely toxic and if they do cause problems it is typically only mild GI upset.
